The world’s smartest hospital
As Hospital Director of Oulu University Hospital, Dr Miia Turpeinen is intricately involved with the €1.6 billion project to build ‘the world’s smartest hospital’ in the city of Oulu, Northern Finland. Here she describes the vision, planning and innovations adopted by this brand-new cutting-edge hospital in one of the world’s leading public health services
The new Oulu University Hospital in North Finland is a teaching hospital which serves a large geographical area – over 50% of Finland. The project began in 2012 with a plan to renovate our old, dilapidated hospital, but by 2018 we realised that it would be more efficient, sustainable and cost-effective to build a brand-new building at a cost of €1.6 billion.
We make the bold claim that it will be the smartest hospital in the world when it is fully operational in September this year. It’s not just about new technology – although that’s an important part of its functioning – our vision is also focused on creating more patient-centred care and better meeting the needs of our staff so we can boost retention.
To do this we had to change some of our ways of working. In the past, we would have implemented these changes with old-style thinking – namely that we, as leaders, know what is best for our patients and staff. But this time we approached it differently, asking the patients, staff and students what they needed and wanted in more than 500 specially designed workshops. We consulted them about treatments, processes and the design of the new hospital.
Our vision for change is that the newest technologies, modern facilities and up-to-date expertise will combine to ensure effective and influential care that is the best in the world.
But a smart hospital is also client and patient orientated. The patient is treated at the right time in the right place humanely and effectively and without unnecessary delays.
Patient-centred care
In the past, we’ve tended to think of patients as objects rather than subjects, and assumed they wanted all the available and latest treatments. But when we talked to patients, we learnt that often they valued different aspects of their care.
For example, in oncology, there used to be this philosophy that you need to give every single available treatment. But when we asked patients what they wanted for the last months of their lives, what they valued was being at home, not being in pain, and not feeling sick so they could function.
Now we try to measure the holistic value of our treatments. So rather than measuring how many procedures we’ve done, how many times patients have visited us, or how many times they’ve used beds, we’re asking did the treatment add value to their everyday lives?
Another example might be orthopaedic surgery: we might recommend a hip replacement, but the value of the operation should be measured by patient outcomes. If there is still a need for painkillers and difficulties in walking afterwards, the procedure cannot be considered very successful or valuable, although the operation itself might have been technically perfect.
Tech innovations
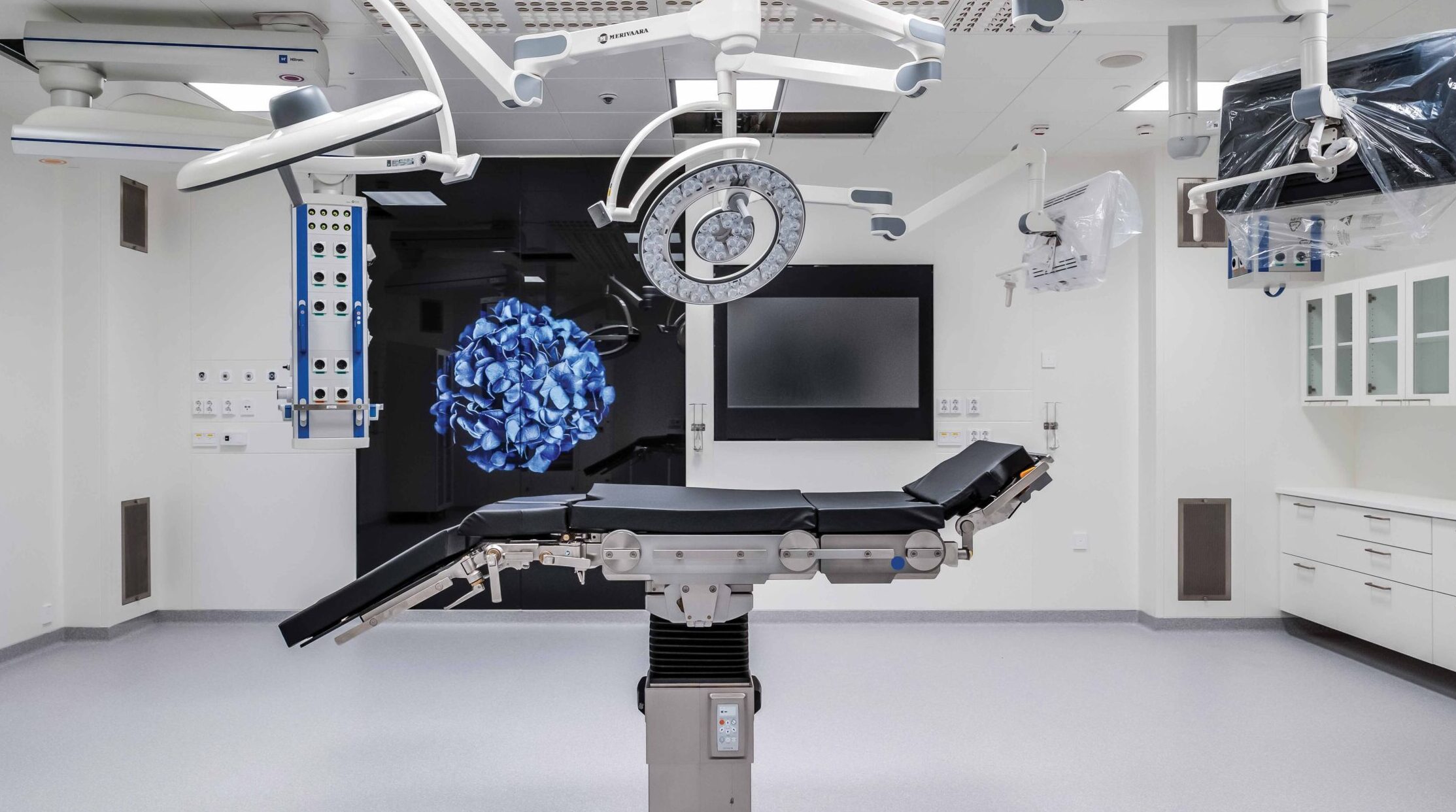
We have all the latest technologies, such as robots in operating theatres. But one innovation we are particularly proud of is the ‘closed loop medication administration’ (CLMA) system. This is a digital drug distribution pathway which cross-checks the correct patient, medicine and prescription using digital technologies. It was one of the first technologies we implemented and is already massively reducing the number of human error mistakes, and the number of patients impacted by avoidable harm. It also benefits the staff by freeing up their time.
We’ve also put in place digital care pathways to complement traditional healthcare and appointments, and we think we have one of the best systems in the world. Here’s why: the idea is that the patient doesn’t need to continuously be on the move – information moves, the specialist moves, and knowledge moves. Patients can go online and fill in surveys related to treatment and receive feedback on them. They can send follow-up information on symptoms and health check-ups to the professionals treating them and communicate with them via messages or remote appointments. We cover such a large geographical area that this works for us, and we’ve discovered that young people, in particular, are very happy to have the flexibility of medical appointments wherever they want.
Of course, this is not for everybody, but what it does is free up time for those who need in-person contact. When more tasks are automated, there is more time for hospital staff to meet patients in person. Some older people might prefer to see a doctor in person, but we’ve found even older Finns are quite proficient at using apps and digital services. The majority own a mobile phone and there are community services, such as libraries, where they can go if they need help.
“Technology also helps us to be minimally invasive, as we can utilise robotics and focused ultrasound and monitor patients with remote monitoring technology – such as the system from Philips Healthcare – when they have been sent home. Our broader goal is to increase the number of outpatients as opposed to inpatients and improve our links and integration with the wider areas.
Clinician-centred care
We designed the hospital together, not just with the current staff, but we also consulted the students and nurses who are hoping to work with us in the future – they have the best ideas! We listened to what they said they value, like work/life balance, for example.
When we talked to staff, they told us that departments were too far away from each other, and it was hard for them to work closely with each other and share information. As a result, our new hospital is 10% smaller than the old one, we have fewer beds and departments are closer together. We are one of the few hospitals in the world that is downsizing and yet we aim to improve productivity by 10-15%. When we’ve tested the new buildings, we’ve seen that staff are sharing resources more effectively, and we have special areas where they can hold impromptu discussions. They’ve told us that this has produced a broader knowledge base where, for example, cardiologists and thoracic surgeons can share knowledge. This gives staff a greater chance to learn and grow in their work and is much more motivating for them.
Of course, our old facilities were also in very bad shape, and the new building is also a key motivator for our staff.
The design and build
Many old hospitals have historical and cultural value, and our original plan was to renovate our old hospital, yet what we learned was that it’s hard to operate 2024 technology in old facilities. It was going to cost €300 million more to renovate the existing building, and the old space and structures wouldn’t have provided a framework for more efficient nursing care. With the new building, we have saved money and time as it can be completed years faster.
Building a new hospital also meant we could focus on sustainability. We’ve reduced our energy consumption, improved ventilation, covered the building with district heating. With district heating, the heat is generated in a central facility and then distributed through a large network of insulated pipes. A heat pump is used to produce the year-round cooling and the condensing heat from the heat pump is used in the building system. This condensing heat would normally go to waste, but in our system it is used for heating and hot water – an eco-friendly and cost-effective solution.
Environmentally friendly heat generation is constantly being developed, and by 2035 all the district heating will be completely carbon neutral, which is particularly important for a cold Finnish winter.
We’ve also made the patient rooms bigger so that, if they want to, patients can have a family member stay with them, so they are not alone, which they told us was a key concern. To create more space for patients, we’ve also reduced other areas. We don’t have a great hall as you enter the hospital, for example, as it was considered a non-productive area. Our design focused on patients’ needs rather than the architects’ desires.
Communicating with stakeholders
How do you communicate with everybody when the audience is everybody, as it is in the case of a large public building and service such as a teaching hospital? That’s a crucial question, and we realised that it’s not something you just bolt on – it is vital it is operational all the time. So, we have newsletters, press releases, intranet pages, social media, and also co-creation where staff and the public have the opportunity to participate actively by submitting ideas, for example through the public innovation form.
We’ve gone to all kinds of events and marketplaces and asked people what they think. It’s taken a lot of time and people, but it’s important because this is a public hospital and it’s for everyone, so it’s not for us to keep all the information to ourselves.
Funding, finance and politics
The hospital is entirely funded by government taxpayer money. Of course, it had to be evidence-based, but we were able to show that this would save money in the long run and add value to the users of the hospitals, so I think our politicians saw the value and reasoning behind it.
Patience is required for a major project like this, and you need people to consistently back you. Our politicians have given us time and space. Of course, they will expect us to evaluate the hospital when the time is right, but they’re not interrupting us. I think it’s good to operate this way; if you are always being placed under annual review then it can lead to fixating on the wrong things, or in the worst-case scenario a kind of ‘fix the stats’ approach.
Lessons for the NHS
The most important lesson is that co-creation is the key to our success – it’s something we’ve done well. Another element that we have been happy with has been the alliance model. We have built the hospital through co-operation using this model from builders, funders and users – everybody has participated together so that it’s a mutual win-win. If there is a problem, it is everyone’s problem, and we solve it together and look for solutions, rather than blame each other. I couldn’t imagine building a hospital the old-fashioned way again.
Future planning
We are horizon-scanning all the time. We test and assess continually to decide whether there is a new technology available, asking if the evidence is there for it to be introduced, and should we do away with old ways of functioning. This is a key part of our project too – being flexible and moving with the times.
Above all, we are a community made up of patients, family members and relatives, as well as personnel, and we work together holistically and humanely. We aim to keep looking into the future to learn and grow continuously.
© Dialogue Content Marketing Ltd 2025.
This article was taken from the May 2024 edition of FORTIS magazine.
FORTIS magazine is a Health Spaces Limited publication. Opinions expressed in FORTIS magazine are not necessarily those of Health Spaces Limited or Dialogue Content Marketing Ltd. Material contained in this publication may not be reproduced, in whole or in part, without prior permission of the publishers. No responsibility can be taken on behalf of advertisements printed in the magazine.
FORTIS magazine – read more
This article was written for the November 2024 edition of FORTIS magazine; a forum for the NHS to share ideas, innovations and case studies. To read the publication in full and access digital copies, visit FORTIS magazine. FORTIS magazine is free for NHS change-makers and leaders and is available as a print or digital copy. FORTIS magazine is managed and owned by Health Spaces Ltd.